If you are new to the blog, I invite you to read the introductory post here.
In my previous post, I shared part of the findings from the investigation conducted by the patient experience department at the hospital. This investigation centered around my complaints and requests I submitted. There were several responses the director shared regarding my complaints that were completely false. And, of course, the hospital refused to honor any of my requests. One of which was my suggestion that a more detailed consent form be implemented that contains a provision for a patient to consent to intimate procedures, such as what I endured when my disposable underwear was cut off and my pubic hair shaved for a procedure involving incisions around my knee.
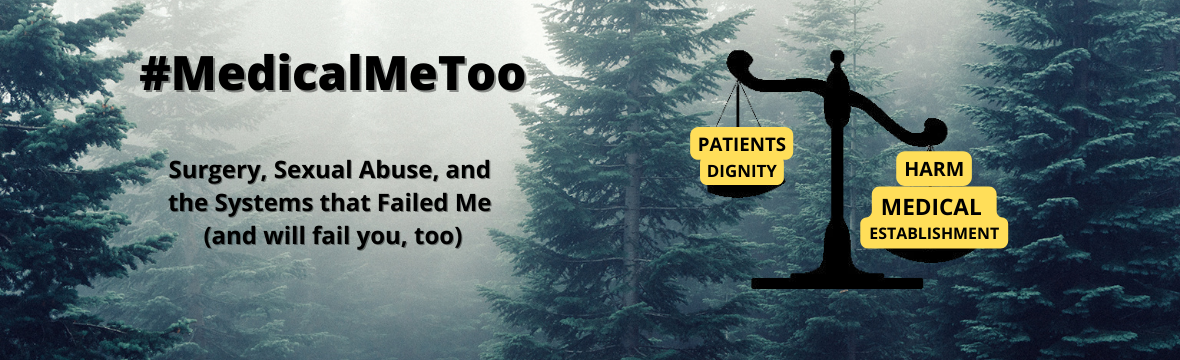
Doctors are required by law to obtain consent for procedures. Without it, they are committing assault. Therefore, it follows that without expressed consent for intimate procedures, medical staff are committing sexual assault. Or it should be. There are reasons why there are laws specifically dealing with private areas of a person’s body. So there should be specific provisions in medical consent forms dealing with private areas of a person’s body as well. But there isn’t. While I have been encouraged by the increasing number of states passing laws banning non-consensual pelvic exams. The result has been updated consent forms. But these laws and consent forms don’t go far enough. So I have been advocating for consent forms that protect all patients for all procedures against any unwanted and non-consensual intimate experiences for elective procedures. You would think this shouldn’t be a problem if medical personnel truly respect a patient’s personal dignity and humanity. But apparently it is.
When the director of patient experience investigated my request for a more detailed consent form, the hospital responded with this:

So they think it is appropriate to withhold information from patients regarding private areas of their body being involved in a procedure. And it is acceptable to do this even though they know well in advance that intimate tasks will be performed on patients. In other words, they are admitting that it is acceptable for them to choose to withhold this information from patients and drug them out of their minds while these intimate tasks are being performed without their knowledge or expressed consent. They adhere to the philosophy of “What they don’t know won’t hurt them.” This is far from the truth. It does hurt us. Some of us end up developing mental health issues that rape victims experience. So if they truly cared about our well being, they would obtain expressed consent for these intimate tasks they are performing while the patient is drugged and unable to defend himself or herself. But it’s just easier for the medical personnel because they don’t have to deal with “back-talking,” “non-complaint,” “difficult,” and “defiant” patients who only want to the right to determine what happens to private areas of their body. Patients only want to preserve their personal dignity, modesty, and humanity. Denying patients this right is about power and control to the medical community.
The nonsense about them taking my suggestion into consideration and appreciating my recommendation is just that: nonsense because they also think their consent process is appropriate.
I asked the director of patient experience to relay my request for the hospital to reconsider their denial in implementing a more appropriate consent form that includes intimate tasks. The following is the correspondence I obtained between the director’s office and the head of the vascular surgery department:

So then, a member of the patient experience department contacted the head of the committee. The following is his response:
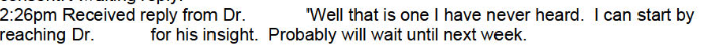
Talk about how completely invalidating the first sentence is. I can picture him laughing at the request. He didn’t have to make that comment, and he may not have if he knew I was going to have access to this conversation. But then again, he may have. This just shows how out of touch medical personnel are when it comes to intimate tasks. As I shared before, there are a number of reasons why patients would not reveal distress after being stripped naked and having intimate areas of their body viewed and contacted. They include: intimidation/power imbalances, shame, embarrassment, fear of retaliation from the provider, fear of invalidation, lack of trust, machismo in the case of a male patient, etc. Some may try to erroneously rationalize it as “That’s just the way it is.” Some may be afraid to be labeled a “prude.” Some may feel hopeless, or that it would be pointless to complain out of the belief of nothing ever being done. All of these reasons lead to patients suffering in silence. Therefore, providers often do not know what trauma, stress, and anxieties they have caused their patients. And it is unnecessary and avoidable.
This doctor’s response of “Well that is one I have never heard” is all the more reason why more patients need to complain and continue complaining until our voices are heard.
By the way, the doctor he referred to as the guy he planned to reach out to for insight was the head of the vascular surgery department – the guy who I noted in the previous post that prep is determined by an automated process. This is also the guy who just told the patient experience department in the email above that implementing a supplemental consent form dealing with intimate access was not his call and to contact the head of the surgical services committee. So it’s almost as if they are deflecting blame and passing the buck.
In the end, this is the official response I received from the patient experience department:

The last sentence seems to make it seem as if they were blowing me off. It’s been over a year and a half since they claimed to consider my request, and I still have not heard whether they implemented a more comprehensive consent form that includes intimate access of a patient’s body. But given that they consider their current consent process appropriate, that the head of the surgical services committee seemed to mockingly comment that he had never heard of such a request, and that he and the head of the vascular surgery department seemed to be passing the buck, I’m not holding my breath of them actually implementing a policy requiring providers to reveal to their patients that they will be visually and physically accessing intimate areas of their body that are not directly involved in a procedure They like their power and control too much. Seeing how it has taken legislation to get the medical community to stop performing non-consensual pelvic exams on women, it is quite apparent that they have no interest in policing themselves.
In asking providers to seek consent for intimate tasks that will be performed, I feel as if we are peons begging our powerful handlers not to harm us, or, more appropriately, rapists not to violate us.
After receiving the director’s notes with the hospital’s responses to my complaints and requests, I then asked him to address the violations of my bill of rights. All hospitals, by law, have to communicate a patient’s bill of rights, which I will discuss in a subsequent post. The director responded by telling me to direct all future questions to the attorney general’s office.
With the one-year anniversary approaching and no accountability in sight, I decided to escalate my complaints. The hospital clearly wanted me to just go away. So I contacted campus police.